Hot 96.7 Shows.
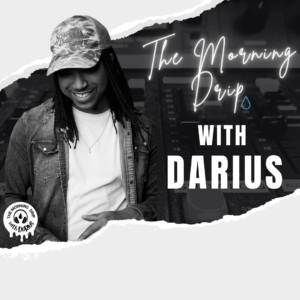
The Morning Drip with Darius
6AM – 10AM Weekdays

Blair – The Morning Drip with Darius
6AM – 10AM Weekdays

Middays with Stunt Monkey
10AM – 3PM Weekdays

Afternoons with Mollywood
3PM – 8PM Weekdays

Weekend Throwdown
4PM Sunday Nights
join us on social.